CAPITOL HILL
House, Senate leaders prep a pile of health bills
House and Senate committees are drafting their next set of health care bills, with some hope that they can garner ever-elusive bipartisan support by targeting favorite bogeymen in the health costs debate.
That includes legislation in the Senate aimed at pharmacy benefit managers and drugmakers' patent thickets, plus measures designed to to boost generic drug competition, according to four lobbyists who spoke to my colleague John Wilkerson (Axios first reported Senate talks).
In the House, health committee leaders want to tackle transparency in hospital costs, a priority that E&C Committee Chair Cathy McMorris-Rodgers signaled early in her tenure and with a recent hearing. Lobbyists tell D.C. Diagnosis that transparency measures — designed to get hospitals actually complying with Trump-era price rules — could get tied into a larger affordability package with Democrats' buy-in. But it's still early days, and if the recent QALY bill debate is any indicator, bipartisan bills can fall apart fast.
INSURANCE
A modest Medicare Advantage move
CMS late Friday quietly announced a smaller-than-expected pay cut for Medicare Advantage plans and a three-year runway for coding changes designed to rein in costs, dramatically softening an initiative to reverse years of overpayments to commercial insurers after intense industry lobbying, as my colleague John Wilkerson reported Friday.
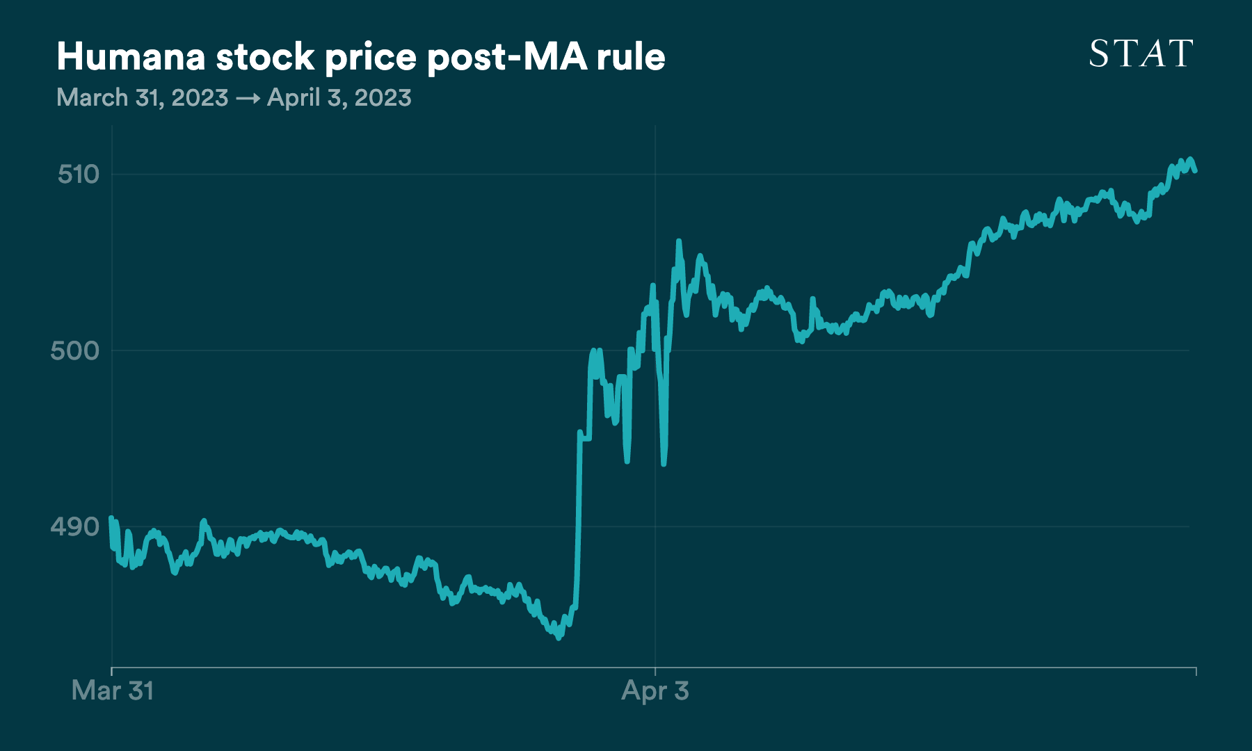
The agency will decrease baseline payments by 1.1%, up from the 2.3% decrease previously proposed — but payments will be higher after factoring in how plans code their members' illnesses. And while it will eventually consolidate some treatment codes to prevent Advantage plans from overbilling the government on sick patients, skeptics say the three-year timeline gives plenty of room for insurers to make changes that protect their bottom line. If you had any doubt of whether the delay benefits the insurance industry, look what happened to the stocks of the biggest MA players yesterday. Humana, for instance, represents 18% of the MA market according to KFF, and:
The government still plans to aggressively audit Advantage plans, but that might not deliver savings for a while. Meanwhile, CMS said in updated projections Friday that traditional Medicare spending will go up 2.3% in 2024 and said the program's trust is solvent until 2031. While that provides a few years' more padding than the agency projection last year (lasting until 2028), it relies in part on projected savings from Medicare Part D negotiation that hasn't been finalized.
WHITE HOUSE
Biden officials: Please, fund our cancer efforts
HHS on Monday released a National Cancer Plan that essentially reiterates President Biden's relaunched Moonshot — to halve cancer deaths and curb new cases — but without mentioning the billions of dollars the president requested to fund those goals in 2024.
The eight-point, 25-page plan rehashes Biden's goals of catching cancer early through screenings, curbing new cases through preventive education and improving data and care. Awkwardly, it comes just days after a Texas federal judge struck down an Obamacare provision requiring insurers to cover a range of cancer screenings — a decision HHS is appealing. It's not in the new National Cancer Plan, but in its 2024 budget proposal the agency has asked for $3.6 billion to refill the Moonshot's coffers, on top of more than $7 billion for the National Cancer Institute and another $2.5 billion for the Advanced Research Projects Agency for Health, which could fund cancer research projects.
"This is a sensible plan, an achievable plan," Karen Knudsen, CEO of the American Cancer Society, told DCD. But at the same time, "we need to erase some of these unnecessary barriers," she said. "The data tell us without question, unequivocally, that copays are barriers to cancer screening."


No comments