Pixel tracking
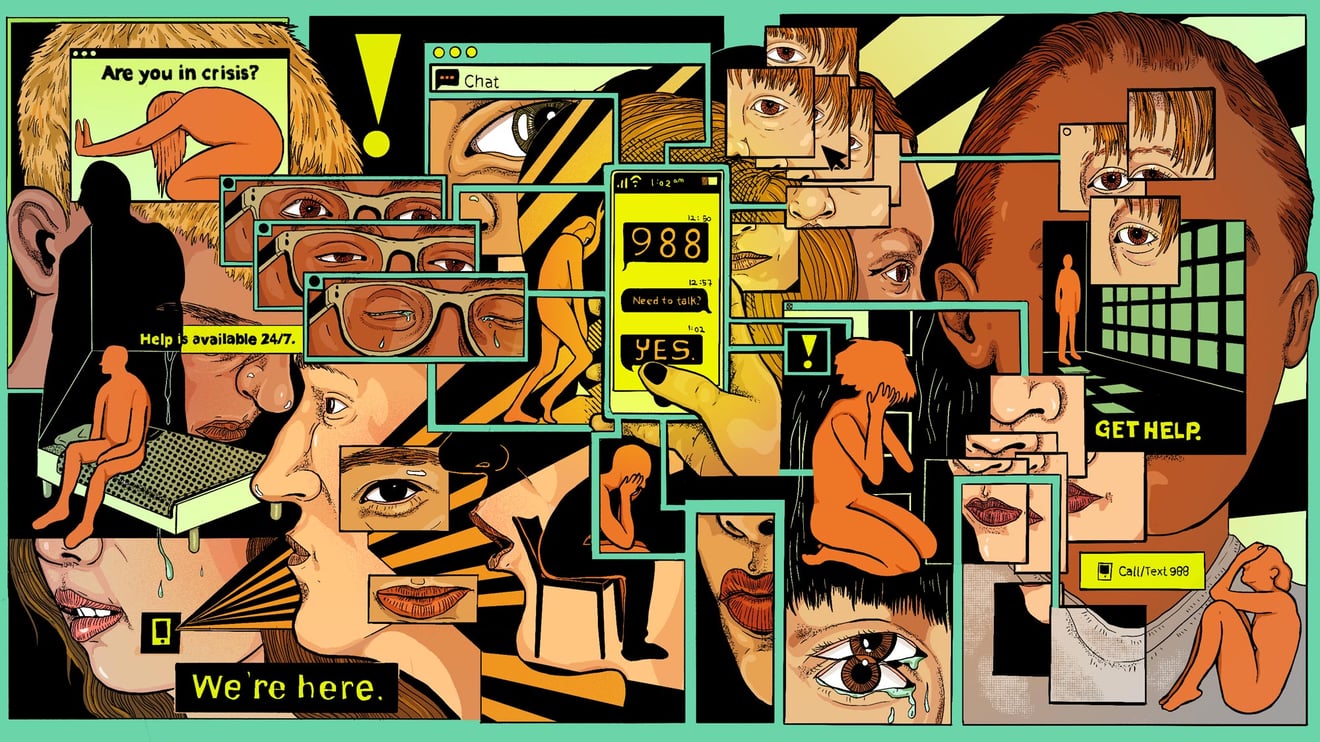
Suicide hotline websites promising anonymity are sharing data with Facebook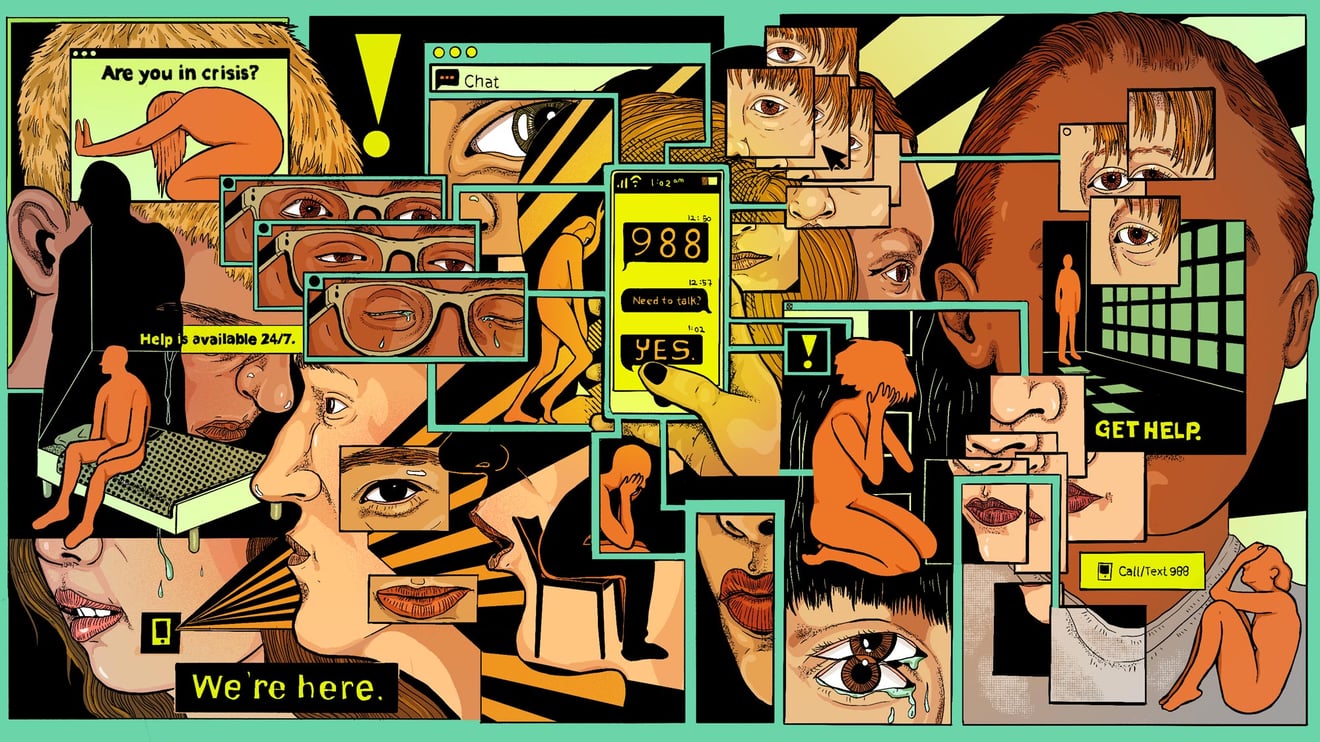
Websites directing people in crisis to mental health resources are also quietly sharing sensitive data about visitors with Facebook, The Markup's Colin Lecher and Jon Keegan report in an investigation co-published with STAT. Those websites, linked to the national crisis hotline 988, use a Meta Pixel tracker, which gathers data about website visitors and shares it with Meta in exchange for detailed analytics. The analysis of 186 local crisis center websites found the shared data often included signals to Facebook when visitors clicked on dedicated call buttons for mental health emergencies. In some cases, users' contact information — including names and email addresses that could easily be unscrambled — were also transmitted. Read the full investigation here.
Health systems
Providers using AI weigh what to tell patients
I spent last week canvassing health systems across the country — spanning from New Jersey's Hackensack Meridian Health to UC Davis and UC San Diego Health — on their plans for generative AI. Most said they're taking things slow, testing and re-testing tools out in sandbox environments, or offering the tech only to providers and administrators who can vet their content. Despite unprecedented momentum surrounding generative AI, leaders told me they're extremely wary of any patient-facing applications until they're sure the AI won't hallucinate.
Still, a handful are pushing ahead with generative AI tools designed to to help doctors respond more quickly to non-emergency patient messages. I asked how they disclose their use to patients, and found that there's still no industry-wide consensus on what to tell patients about AI. Some likened AI-guided drafting to email templates; do patients need to know about productivity tools doctors use?
Harvard's I. Glenn Cohen said health systems are weighing the risk of alarming or overwhelming patients with technical explanations against violating their expectations for the doctor-patient relationship. But "if you think it would really matter to patients, what justification do you have for withholding this information?" he said.
Let me know how your health system approaches this, and read more here.
From the bay
Uber Health expands into groceries, OTC items
The ridesharing giant's health division will soon allow providers and insurers to order groceries and over the counter items for patients, in addition to the non-emergency medical transport and prescription delivery it already offered, the company announced today. It's Uber's bid to integrate more deeply into traditional health care settings by knitting together services that health insurance might cover, global head of health Caitlin Donavan told me.
Donavan said the announcement is the culmination of years of working to address the hurdles patients face getting healthier — beyond just making it to appointments. "We now have a one stop shop that allows [providers and payers] to connect patients to the things they need, and are covered by insurance."
Care coordinators — whether they're social workers, clinicians, or health plan workers — can call up these services through a web dashboard where appropriate, Donavan said. "Too often, health plans create a benefit and don't think about practically how patients will access it," she said.
Washington
Medical device reimbursement rule makes progress
Device lobbying group AdvaMed met with the Biden administration yesterday to talk about a forthcoming Medicare rule that would create an easier reimbursement path for breakthrough medical devices, my colleague Lizzy Lawrence tells us. The industry's hope is the regulation will help founders tackle the "valley of death" between FDA approval and the struggle to secure coverage from health insurers.
CMS sent a notice of the proposed regulation, dubbed "Transitional Coverage for Emerging Technologies," or TCET, to the Office of Management and Budget on April 28. It's unclear when it will be drafted and released publicly.
TCET is meant to replace a Trump-era rule that would have automatically given four years of Medicare coverage to devices granted breakthrough status by the FDA. In 2021, the agency rolled the Trump rule back to account for CMS having a different, and typically higher, data standard for devices when compared to the FDA. Top CMS officials claimed to be working on a replacement in a 2022 JAMA editorial, and device makers have been eagerly awaiting the new rule ever since. Some lawmakers called CMS out at a Ways and Means meeting last month for taking longer than their planned April release date.
A version of this also ran in STAT's twice-weekly DC policy newsletter. You can sign up for that here.





No comments