STAT investigation
The war on recovery: How the U.S. attacks the best weapon we have against opioid deaths
Thumy Phan for STAT
They are not perfect, but they are the best tools we have: Methadone and buprenorphine are highly effective at preventing overdose deaths. They're cheap, they're easy to use, and they work. But these drugs, forever tarnished by a former head of Health and Human Services calling their use "just substituting one opioid for another," reach barely one-fifth of the roughly 2.5 million Americans with opioid use disorder. That means tens of thousands have died for lack of it, blocked by stigma and barriers to access.
This failure is an active choice, STAT's Lev Facher learned in a yearlong investigation. Virtually every sector of American society is obstructing the use of medications that could prevent tens of thousands of deaths each year. That includes Narcotics Anonymous, rehab facilities and sober living houses, regulators of the trucking and airline industries, and medical boards that restrict doctors and nurses in recovery from taking the drugs they'd prescribe to patients for opioid addiction.
"We have a tool, medication-assisted treatment, that we know dramatically reduces overdose deaths," said David Frank, a medical sociologist at New York University who is in recovery from opioid addiction and takes methadone. "But because it's so difficult to access, people that could and should be alive continue to die."
"
"I estimate that we would have at least 50% less people dying, and that's conservative. I think it would probably be much more consequential."
Nora Volkow
director of the National Institute on Drug Abuse
Instead, we have painful and ineffective "detox," horseback riding, or 12-step approaches.
"While such programs rely heavily on hope, mindfulness, and religion, they often ignore the physiological realities of addiction — in particular, the debilitating withdrawal that occurs when regular opioid users attempt to suddenly stop," Lev writes. "In any other medical field, favoring prayer over proven medication would be considered malpractice. Yet for addiction treatment in the U.S., it's simply the way things work."
Read more about how the two medications work, how hard they are to get, and what other countries do to enlist them in recovery. Lev quotes Kurt Cobain and Alex Hogan's video explains the nightmarish reality of withdrawal. Don't miss Lev's Q&A with Nora Volkow, who has been director of the National Institute on Drug Abuse since 2003.
covid's long tail
Large study finds the risk of an autoimmune disease rises after Covid infection, but wanes
In yet another impact of Covid-19, infection with the virus appears to raise the risk of developing an autoimmune disease, a large study from South Korea and Japan suggests. The paper, published yesterday in the Annals of Internal Medicine, found that among 22 million people studied from 2020 through 2022, there was a 25% greater risk among those infected vs. not infected of developing such autoimmune diseases as rheumatoid arthritis, systemic lupus erythematosus, Sjögren syndrome, mixed connective tissue disease, and vasculitis. Compared to people who had contracted the flu, the Covid risk for autoimmune illnesses was 30% higher.
The researchers did find that being vaccinated against Covid lowered the risk of developing an autoimmune inflammatory rheumatic disease, possibly because vaccination protected them from more severe disease. And the risk dissipated in the year after Covid infection, raising questions about whether what looks like autoimmune disease is a temporary flare of the immune system. STAT's Isabella Cueto has more.
health
How infant mortality rates vary by race and other characteristics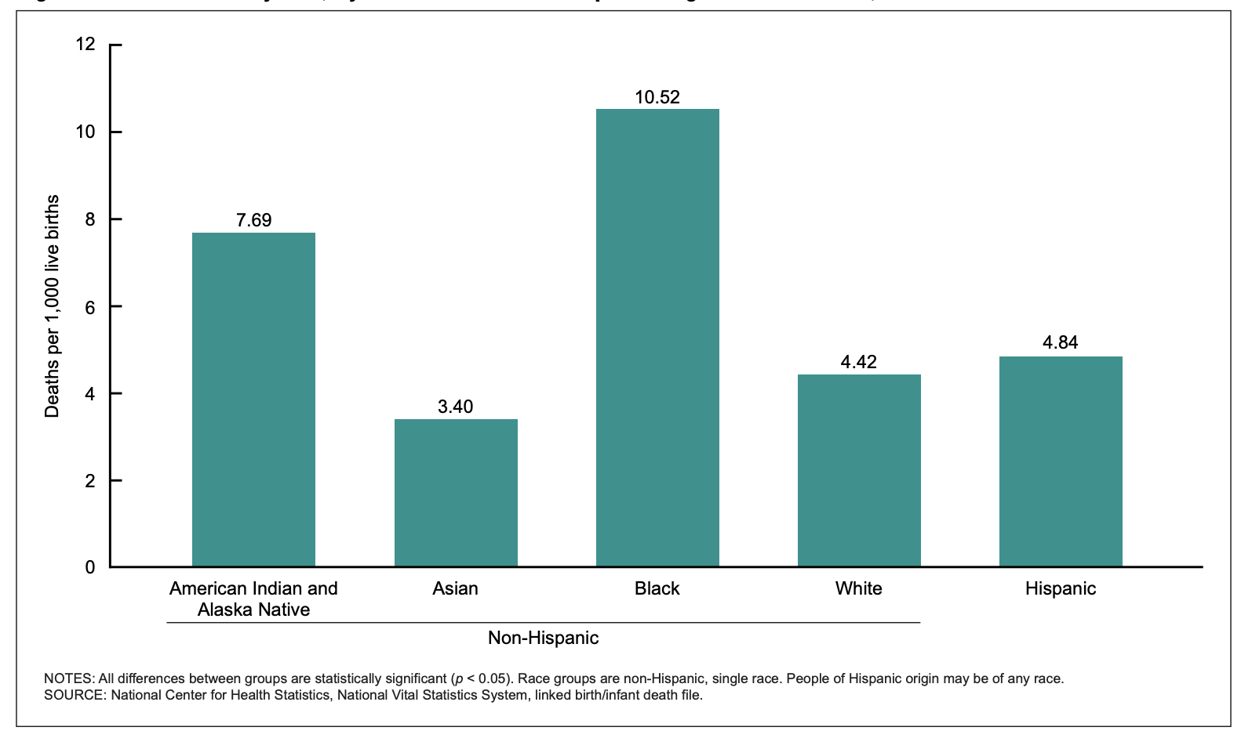
NCHS / CDC
Infant mortality grew by 3% in 2022, the biggest increase in 20 years, the CDC reported in November. Now, a new analysis led by the same researcher looks at how rising rates vary across race and Hispanic origin, combined with certain maternal characteristics.
Mortality rates in the first year of life continue to be higher for infants born to American Indian and Alaska Native women and to Black women, while they are lower for Asian women. Overall, mortality rates were highest among infants of women with obesity, women who smoked, women who received the WIC nutrition benefit, women who began prenatal care later in pregnancy, and women covered by Medicaid. There were some differences:
- Infants of white women who received WIC had higher mortality rates than infants of white women who did not receive WIC. The opposite was true for infants of Black and Hispanic women.
- The percentage of women with obesity was higher among American Indian and Alaska Native and Black women than other groups.
"Some of these characteristics can be used as proxies for societal inequities by race," the authors conclude.


No comments