medicine
How telehealth providers can drive antibiotic overuse
More than a quarter of outpatient antibiotics are inappropriately prescribed, and as STAT's Katie Palmer writes, telehealth could exacerbate the problem: Studies have suggested that virtual visits, on average, result in more antibiotic prescribing than in-person visits. But not all telehealth is created equal — and research is beginning to untangle which approaches are more likely to result in unnecessary antibiotics. In turn, national telehealth guidelines and standards are fighting back by prioritizing safe and effective virtual prescribing practices. These questions come amid bubbling concerns about the safety and necessity of telehealth prescribing in general.
Read more here
policy
Lawmakers huddle on telehealth bills
The House Energy and Commerce Subcommittee on Health is considering more than a dozen bills as it races to beat the December 31 expiration date for some pandemic virtual care flexibilities, such as easing requirements for the patient's location during telehealth visits. With mountains of data from the past few years on telehealth's impact on cost, fraud and safety, lawmakers appear closer than ever before to establishing more permanent policies.
My colleague Mohana Ravindranath tells us that during a hearing yesterday, Health subcommittee chair Brett Guthrie (R-KY) acknowledged that fraud and abuse cases haven't proliferated in telehealth as much as critics expected, citing recent data from the Health and Human Services Department's Office of the Inspector General. "It appears that telehealth can be used to deliver care without actually raising those serious concerns," he said.
Cost, however, could still be a hurdle in Congress. Permanently extending telehealth flexibilities is likely to cost more than the $2 billion, according the Congressional Budget Office estimate for the previous extension, Guthrie said.
And lawmakers still must also grapple with state licensing restrictions that prevent clinicians from treating patients while they're traveling, for instance.
"Right now, it's creating a lot of a chilling effect, where Physicians are worried that I don't want to abandon my patient, but I am risking my license by caring for them and providing advice over the phone or a over a video visit," said Ateev Mehrotra, a Harvard professor and frequent Congressional witness whose research has often challenged telehealth advocates' assertion that virtual care doesn't impact costs and utilization.
Mental health How expiring rule could impact telehealth access
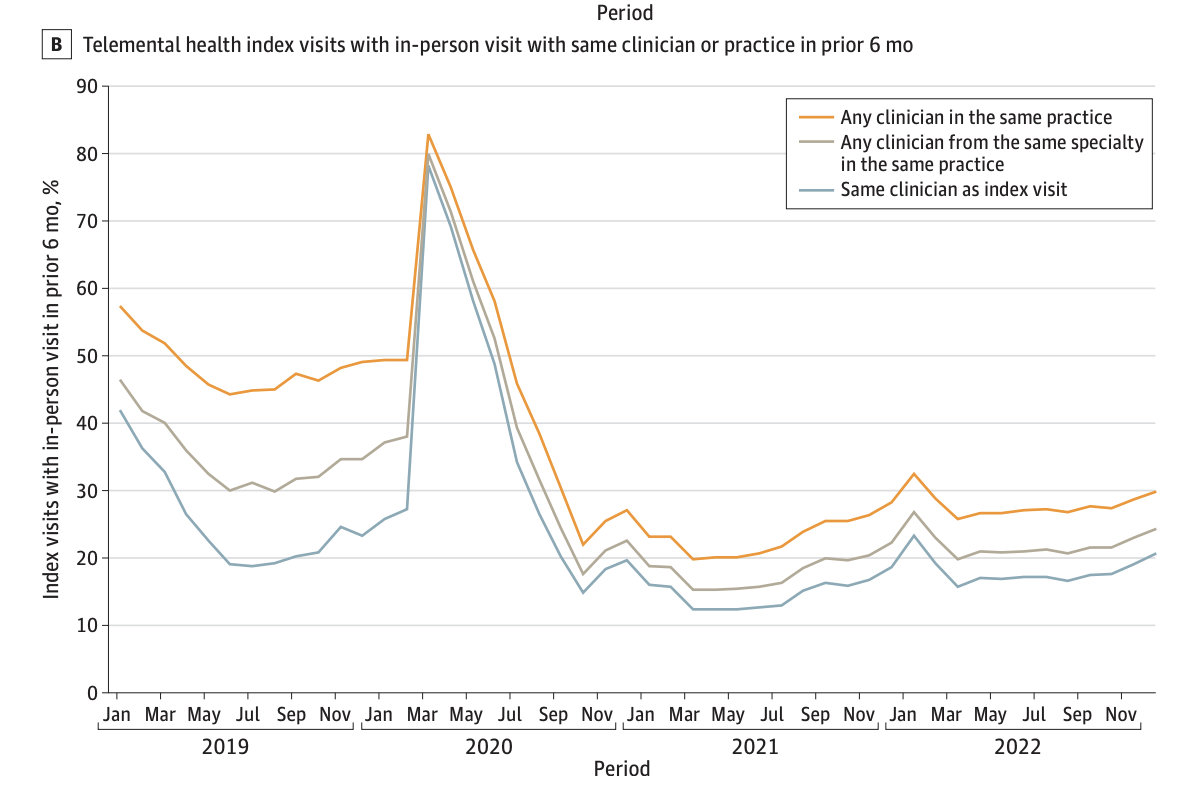
Speaking of Ateev Mehrotra (see above), he has a new paper out in JAMA Health Forum relevant to expiring pandemic telehealth flexibilities — and specifically the currently waived requirement that people on Medicare must be seen in-person prior to receiving mental health treatment over telehealth. Mehrotra and colleagues analyzed initial telemental health visits for people enrolled in traditional Medicare and found that in 2022, after peak pandemic, only about 20% were preceded by an in-person visit. "These findings suggest that Medicare's in-person visit requirement will require substantial
changes in current practice," the authors write.


No comments