Investigation
The quest to remove race from a kidney disease calculator
In a new story, STAT's Usha Lee McFarling and Katie Palmer detail the contentious battle to remove race from a clinical calculator that helps assess the severity of kidney disease. Until recently, estimates of kidney function relied on flawed science to give different numbers to Black patients than others, underplaying life-threatening disease. Thanks to the hard work of researchers and probing questions from patients who wondered why assessments should consider race, the standard practice at most clinics has changed in just a few short years. But not before a few bruising battles that pitted a new generation of physicians with a more nuanced understanding of race against an earlier generation of doctors who were confident in the tools they'd used for decades.
The new story is the latest installment in Embedded Bias, a series where Usha and Katie's explore the use of race in clinical algorithms used in medicine and why it's so hard to take race out of the equation.
Read the latest story here
medical devices
Abbott's latest heart clip data doesn't resolve debate
It was meant as a tie-breaker, but after an Abbott heart clip showed divergent results in two trials, another study doesn't quite resolve the issue. The device, called MitraClip, is implanted to treat mitral regurgitation, a condition where blood leaks backward into the left heart chamber. It was approved by the Food and Drug Administration in 2019.
In newly presented data, people with the device were hospitalized for heart failure less than a control group and scored better on a quality of life measure. But as STAT's Lizzy Lawrence reports, without a reduction in mortality, the results paint a hazy picture of the device's value. Experts said that more research is needed to better understand who benefits the most from the treatment, especially since patients in the most recent trial were less sick than those in previous studies.
Read Lizzy's analysis here
Telehealth A new angle on which docs use telehealth the most
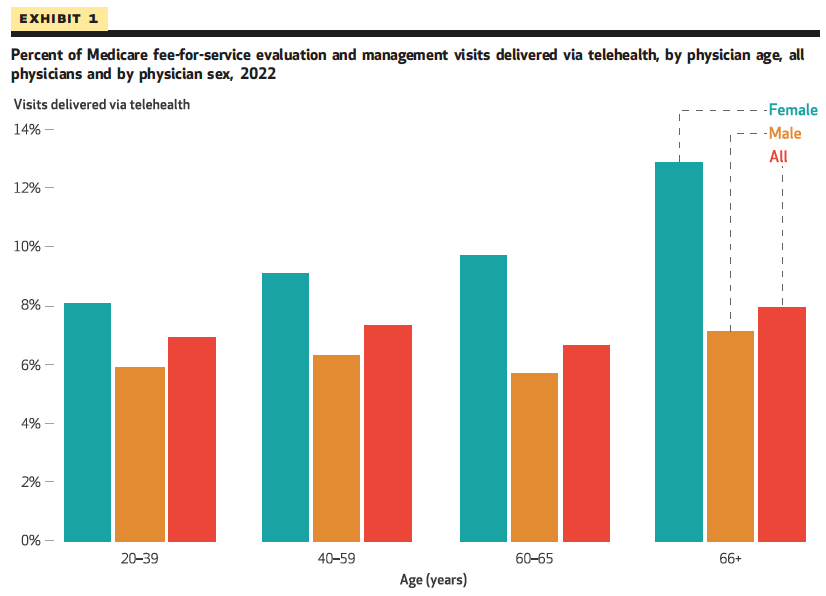
As Medicare telehealth flexibilities rapidly approach their expiration date, researchers from Cornell examined 2022 Medicare fee-for-service claims to understand how physician characteristics impacted telehealth use. They focused on evaluation and management visits, because those lend themselves the most to telehealth compared to visits where there's a procedure.
The researchers billboard the fact that overall, female physicians were "significantly more likely" than male physicians to to deliver telehealth visits. They note the reasons for this warrant more research, but also hazard a guess at an explanation: "It is possible that female physicians, who tend to have greater familial responsibilities, place a higher value on the potential of scheduling and location flexibilities afforded by telehealth." A reach without evidence? Maybe! But to me it is a good reminder that when we talk about utilization numbers for telehealth, we ought to consider not only how technology enables more people to receive care — but also how it potentially eases the burden on physicians who deliver care.


No comments