artificial intelligence
A data point on lagging clinical AI use
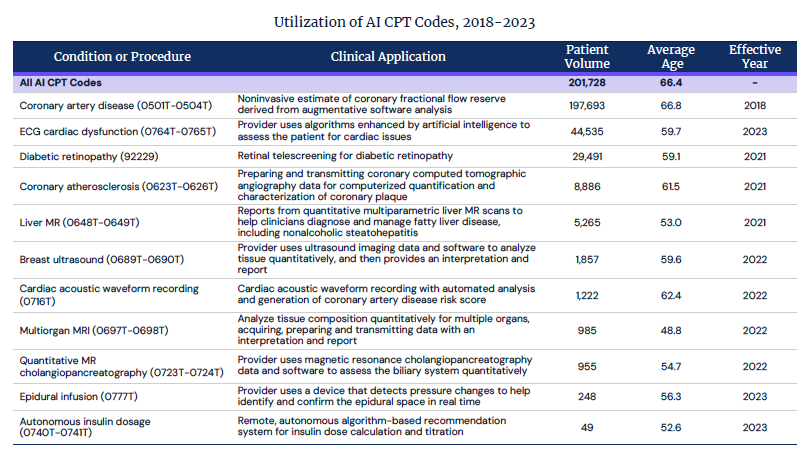
While many people might believe that artificial intelligence tools will make a big impact on clinical care, so far they have landed with a thud, according to an analysis in Trilliant Health's always interesting health care trends report.
Using a very large database of payer claims, the analytics company's researchers looked back at use of the AI CPT codes doctors use to bill for services and found that use has been limited so far: Just over 200,000 patients have received these services. Trilliant's Sanjula Jain said she didn't believe that there was a lot of phantom AI use that wasn't being captured by codes. Fee-based health care incentivizes the creation of codes and billing for services.
"I don't think it's people don't want to bill for it, or don't know that they can bill for it. Because people have lobbied hard to get these codes," she said. "I think it's really a question about clinical utility or clinical value."
Jain noted that this lagging use didn't apply to back office and administrative applications for AI that are increasingly getting the attention of investors, entrepreneurs, and importantly, health care organizations. This gels with other recent findings we recently reported on. (If you think Jain is wrong about clinical AI use, let me know!)
medical devices
ResMed CEO on how wearables, GLP-1s will impact sleep apnea device sales
Earlier this week I interviewed Mick Farrell, CEO of ResMed, the largest seller of continuous positive airway pressure devices that treat sleep apnea. His company has grown to $4.7 billion in revenue and believes it has a lot of head room to grow because only a small fraction of people who might benefit from their devices know they have sleep apnea.
At a fancy event for analysts at the New York Stock Exchange building, the company presented an upbeat outlook. In part Farrell cited what he called "two tidal waves" that would drive patients to the devices: New smartwatch features from Apple and Samsung that alert users that they might have sleep apnea, and the rise of GLP-1s, the wildly popular obesity medications.
Read my story here


No comments