Just in
Health IT regulator changes coming?
Buried in a leaked draft budget from the Trump administration is an ask that may alarm (or elate?) health tech watchers. The administration is proposing to create a new office of the chief technology officer within the federal health department that would house the Assistant Secretary for Technology Policy, the department's health IT regulator, and an "Office of Chief Information." Under the proposal, ASTP would be funded with $9 million, compared to the $66 million appropriated in the 2023 budget.
While this funding document is preliminary and likely to be ignored by Congress (as lawmakers have routinely done in the past), it's notable in light of whispers that a shakeup may be coming to ASTP.
Read more about the budget here and get in touch if you know more.
policy
Radiology network scoops up AI company
RadNet, which runs a network of nearly 400 radiology imaging centers, this week announced a deal to acquire iCAD, a developer of an AI breast cancer screen, for $103 million. RadNet has made a series of acquisitions over the last few years as it seeks to beef up its AI capabilities.
RadNet's willingness to bet big on AI is notable given a tepid response in the market so far. Radiology products account for more than three-quarters of the AI devices cleared by the Food and Drug Administration, but as STAT's Katie Palmer reports, adoption by providers can be bumpy for standalone developers. Reimbursement isn't assured and even then, the economics can be tricky for practices wanting to adopt. An AI used alongside a technician's read needs to make you money, make your practice more efficient, or significantly improve outcomes. Given it's new technology, the evidence of benefits is still emerging.
Read more here
medical devices
Test maker used by UnitedHealth may settle with DOJ
Semler Scientific has offered to pay the Department of Justice nearly $30 million to settle federal health care fraud claims related to its peripheral artery disease test, QuantaFlo. Semler revealed the preliminary agreement in an SEC filing Tuesday. The deal would resolve an investigation into whether federal health programs paid out improper claims based on the use of QuantaFlo, which would violate the False Claims Act.
A STAT investigation last year revealed that UnitedHealth Group, which owns the country's largest Medicare Advantage insurer, boosted Medicare reimbursements by using QuantaFlo to screen patients for vascular disease.
Read more from STAT's Lizzy Lawrence here
research Spending on remote monitoring is on the rise
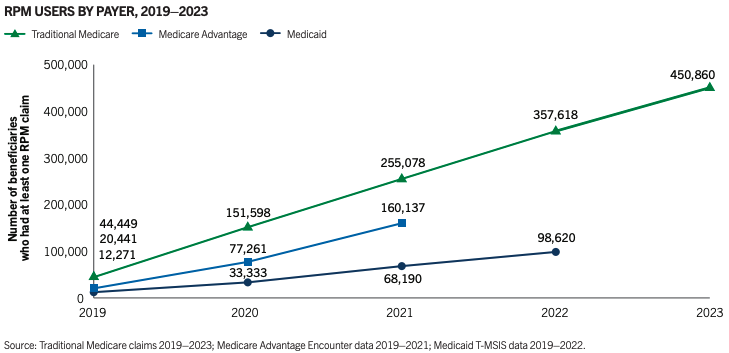
The Peterson Center on Healthcare this week released a report examining remote monitoring technologies, including some new claims data. The chart above shows growing use of remote physiologic monitoring codes, which providers use to bill for setting patients up with devices like blood pressure cuffs and for reviewing the data and communicating with patients about it. RPM spending in traditional Medicare alone has grown from $6.8 million in 2019 to $194 million in 2023.
The center finds there are use cases where remote monitoring has a high clinical impact, like in helping people stabilize high blood pressure. However, the report notes that many of the benefits of monitoring are achieved within a few months and a third of enrollees using RPM are monitored for 7 months or more. The report suggests duration limits for monitoring and limiting payment to conditions where monitoring shows value. Last fall, a federal health department watchdog issued a report warning of the potential for fraud by providers offering remote monitoring to patients.


No comments