policy
CMS proposes updates for RPM, DTx
Medicare regulators on Monday afternoon released proposed payment policies for physician services for 2026, and while we haven't had a chance to parse all 1,800 pages, here are a few initial notes:
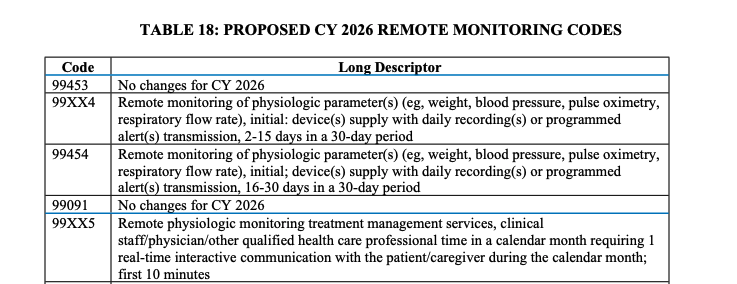
RPM updates: CMS proposed new remote patient monitoring codes that would allow clinicians to bill in circumstances where they collect less data and spend less time interacting with patients, opening the door to more billing. RPM uses include collecting data from a connected blood pressure cuff to help patients get hypertension under control. Currently, doctors must collect 16 days of data per month from patients to bill for supplying devices and are paid for their time only if they spend 20 minutes reviewing data and interacting with a patient. Physicians and industry have correctly pointed out that these thresholds are arbitrary, and last year, the American Medical Association added new codes that allow doctors to bill after collecting just two days of data and 10 minutes of time spent on management. CMS wants to adopt these codes in 2026. There's no world in which this doesn't increase RPM payments, which were over $300 million in 2022.
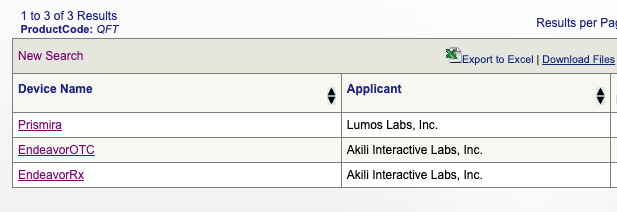
New DTx coverage: Last year, CMS handed developers of FDA-cleared mental health apps a win when it offered a way for physicians to bill for providing the devices to patients — much like how they can bill for RPM (see above). The first pass at policy included only a handful of apps under a specific FDA classification, and industry always hoped it would expand into coverage for more. Wish granted: Medicare is now proposing to cover authorized digital devices for the treatment of attention deficit hyperactivity disorder. Currently, the specific category includes two versions of Akili Interactive's video game treatment for ADHD and a newly cleared digital therapeutic called Prismira from Lumos Labs. Akili famously ran into problems securing reimbursement for its initial product, which was targeted at kids. That brings me to an interesting question: How many people on Medicare will benefit from digital treatments for ADHD? Of the devices CMS proposes to cover, only one version of Akili's product is indicated for people over sixty-five. CMS also invited comments on whether it ought to cover digital therapeutics for additional conditions like fibromyalgia (see: Swing Therapeutics' treatment, Stanza.)
Relatedly, CMS is seeking comments on paying for a "broader based set of services describing digital tools used by practitioners intended for maintaining or encouraging a healthy lifestyle, as part of a mental health treatment plan of care." Is CMS talking about paying for wellness apps?
We'll have more on the fee schedule, as we decipher it. And if you think you know something that we don't, please reach out.
telehealth
Teladoc introduces EAP offering BetterHelp therapy
Teladoc this morning introduced a new employee assistance program offering called Wellbound as the company looks to better integrate its mental health subsidiary BetterHelp into the bigger Teladoc business. The EAP works like many others. It offer members a fixed number of BetterHelp sessions. When those sessions runout, they can continue to pay using insurance, if covered, or by paying out of pocket. Wellbound will offer additional resources "such as legal consultation, access to financial planners and budget specialists, coaching, in-person counseling, and trusted referrals for elder care, childcare and back-up care." Members can also be funneled to Teladoc Health services for psychiatry and other health needs.
BetterHelp earned $1 billion in revenue in 2024, but because it's a direct-to-consumer business, its performance can be a little unpredictable. BetterHelp's been on a downward slide recently. Teladoc's strategy under the new(ish) CEO Chuck Divita includes finding ways to stabilize BetterHelp — packaging its therapy services as part of an offering Teladoc sells to its sizable employer customer base seems a step in that direction. Earlier this year, Teladoc acquired UpLift to speed up insurance coverage for its mental health services.


No comments