Your guide to how tech is transforming health care and the life sciences
| Health Tech Correspondent |
|
|
Good morning health tech readers! Today, we are going to talk about Medicare and technology from four different angles, which are all interesting. At STAT, we are nothing if not thorough. Reach me: mario.aguilar@statnews.com |
|
|
INSURANCE How much AI and RPM should Medicare pay for? Maybe it's just the time of year, which brings fresh fee schedules and insurer medical policies, but we've got two important stories on Medicare payments for health technology. - Beginning in January, Medicare will begin paying over $1,000 for an artificial intelligence product that analyzes CT scans of the heart for signs of harmful plaque that can cause a heart attack or stroke. As more AI products are cleared by the Food and Drug Administration and subsequently covered by Medicare and private insurers, an important question emerges: Are they worth it? Read more from STAT's Katie Palmer on balancing the financial interests pushing for coverage and the need for long term evidence of clinical benefits.
- Elsewhere, starting in January, UnitedHealthcare will stop paying physicians to monitor patient data about chronic conditions like hypertension and diabetes "due to insufficient evidence of efficacy." This includes patients on UnitedHealthcare's Medicare Advantage plans. Industry is in a bit of a huff over the decision, and I'm keeping an eye on how this plays out. Medicare has so far declined to set any guardrails for remote patient monitoring coverage despite increasing use and a growing chorus of voices warning about potential for abuse and waste. Read more in my story here.
artificial intelligence Six companies picked for CMS pilot of AI approvals The Centers for Medicare and Medicaid Services last week revealed the six companies the agency picked for an experimental artificial intelligence-powered prior-authorization program for Medicare, Brittany Trang reports. The pilot, called the Wasteful and Inappropriate Services Reduction (WISeR) model, is a CMS effort to reduce waste and abuse. The vendors picked include venture-backed companies like Cohere and Innovaccer. The pilot will be limited to codes for procedures like skin substitutes and electrical nerve stimulation that have low value evidence or potential for fraud or waste. However, there is push back to the idea that Medicare will use AI to deny care. And there will be an incentive to do so as companies involved will be paid based on "a share of averted expenditures." Read more here
policy How much damage did shutdown do to telehealth? 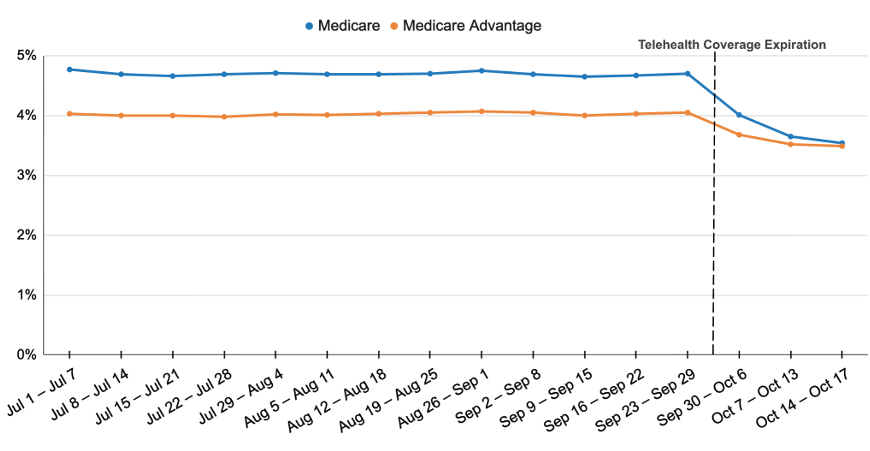
Congress' failure to pass a spending bill at the end of September led to the expiration of Covid-era policies that expanded the telehealth services covered by Medicare. An early analysis from researchers at Brown University School of Public Health suggests an immediate impact. The portion of traditional Medicare visits conducted over telehealth dropped by 24% in the first 17 days of October compared to the preceding three months. In Medicare Advantage, it dropped by 13%. Many providers continued offering services as there was — and remains — an expectation they will be retroactively paid. Overall, telehealth has become a key part of the care for older Americans and other people on Medicare: In 2024, 6.7 million traditional Medicare enrollees, 25% of those eligible, used a telehealth service. Lawmakers seemed poised to end the government shutdown, and the current continuing resolution in the package would once again extend telehealth flexibilities through the end of January. If anything, the last month has showed the precariousness of these short-term extensions tied to funding bills. With more battles ahead, advocates are once again calling on the government to make the Covid-era telehealth flexibilities permanent. Brown's Ateev Mehrotra told me that with continued uncertainty "clinics may be so frustrated by the situation they give up on telemedicine fully." Also subject to new extension is Medicare's hospital-at-home program. Across the country programs were forced to halt ahead of the shutdown. |
|
Health tech news roundup Note: The big Behavioral Health Tech Conference is happening this week, so you'll see a bunch of news related to mental health tech. - Millions of Cigna members will be offered a specialized version of mental health app Headspace that helps them navigate their mental health benefits, the companies announced.
- Virtual mental health company Talkspace announced "Chapters," a new women's mental health offering that "delivers tailored care across women's life stages."
- Amae Health, a startup focused on serious mental illness, raised $25 million led by Altos Ventures to open clinics across the country, "advance its proprietary AI-driven care platform, and support research into schizophrenia, bipolar disorder, and treatment-resistant depression."
- Virtual chronic disease management company Omada reported third quarter revenue of $68 million, up 49% from the same period a year ago. Importantly, the company announced it will finally start prescribing GLP-1 obesity and diabetes medications. The company already offers services to support people adopt physical activity and dietary changes that are indicated alongside the pricey drugs.
|
|
Check out more exclusive coverage with a STAT+ subscription | Read premium in-depth biotech, pharma, policy, and life science coverage and analysis with all of our STAT+ articles. |
|
What we're reading - Q&A: HATCo president on Summa Health's progress, MobiHealthNews
- FDA reverses decades-old warning on hormone therapy products for menopause, STAT
- U.K. releases plan to phase out animal testing in research, STAT
|
|
Thanks for reading! More next time - Mario Mario Aguilar covers how technology is transforming health care. He is based in New York. |
| STAT, 1 Exchange Place, Boston, MA | ©2025, All Rights Reserved. | |
|



No comments